Are you ready to hear what women really think about breastfeeding and pumping in the context of a so-called ‘Baby Friendly’ setting? This recently published paper in the journal Breastfeeding Medicine gives some very interesting insight.
You know the score. The paper starts with the usual creed: breastfeeding has loads of benefits, is a major public health goal and not enough women do it, blah blah blah! Now on to the juicy bit! The authors state that many other studies have sought to identify ‘barriers’ to breastfeeding, but their goal is to analyse thoughts and attitudes towards breastfeeding among women.
We shall see how good they are at putting their listening ears on…
The study surveyed women who had babies in a Baby Friendly accredited hospital in Alabama, 4 to 6 weeks after the birth. The aim was to look at women’s lived experiences of breastfeeding in their own words, and they obtained 110 responses to an open-ended question from 290 participants.
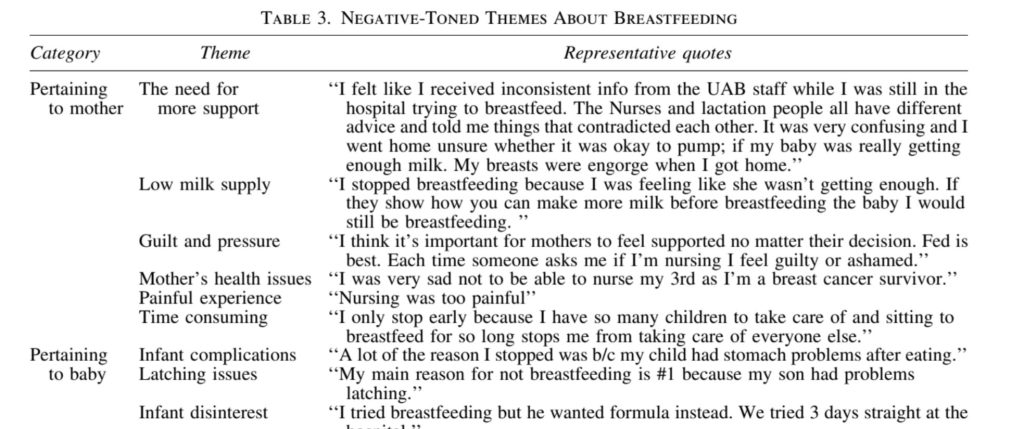
More than half (52%) of participants expressed negative breastfeeding experiences. These included inconsistent advice, low milk supply, guilt, pressure, health issues, pain, finding it time consuming, latching difficulties and disinterest from the baby (tell me again why we are encouraging women to put up with this?)
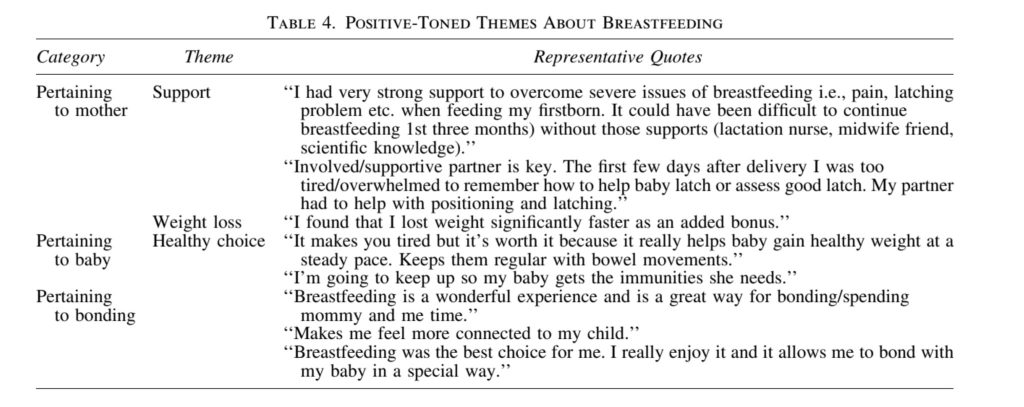
Less than half (41%) expressed positive views. It should be noted that the first positive view here is about having severe breastfeeding difficulties and support to overcome them, which seemed to take three months. Other positive views included the belief in health benefits and feeling bonded with the baby.
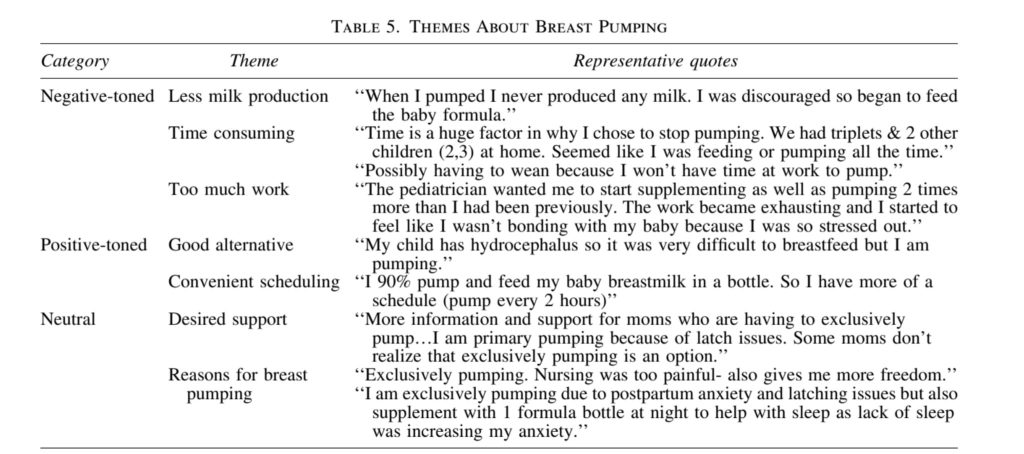
A quarter of participants also expressed views about pumping. Half were positive, half were negative.
None of the content here will be surprising to anyone who is paying attention to infant feeding experiences. Let’s focus on how the researchers interpret the data, because that is much more interesting.
First, and a little surprising to us, they are quite honest that, while women report experiencing breastfeeding as bonding, the evidence on this is inconclusive:
Our view: some women experience a sense of connection when breastfeeding, but this is not true for all and there is no evidence that breastfeeding results in a stronger bond or better emotional attachment or health than formula feeding. We find it refreshing for a paper in this journal to acknowledge the inconclusive nature of the evidence. (Unfortunately, they’re not so questioning when it comes to the health benefits of breastfeeding.)
They frame negative comments about breastfeeding as ‘barriers to breastfeeding’. They don’t consider that these represent adverse effects of breastfeeding, and that women are drawing the conclusion that these adverse effects far outweigh any possible benefits and it is best for them to stop or to reduce breastfeeding.
They highlight the importance of professional, evidence based and consistent lactation advice, but they don’t define what this is. A recent NICE review of the evidence failed to identify any effective interventions that prevent or resolve common breastfeeding problems or assist families to sustain longer term breastfeeding. Right now, what the authors are advocating for simply does not exist.
They recognise guilt and shame when women don’t meet the hospital’s breastfeeding expectations or their own ‘personal breastfeeding goals’:
Let’s be real, hospital expectations are not ‘perceived’. So-called ‘Baby Friendly’ hospitals are explicitly setting out to get more women to breastfeed and to breastfeed exclusively. And let’s talk about breastfeeding goals, shall we? These simply cannot be personal in the midst of breastfeeding advocacy from trusted healthcare providers. And frankly, we question the wisdom of setting a goal for how long to breastfeed or how much breastfeeding to do. Nobody knows in advance what their milk production will be, whether their baby will latch easily, how painful or comfortable or stressful or enjoyable breastfeeding will be. The goals should be good nutritional intake, everyone being comfortable and feeding fitting in with the family’s needs. But this is not research that is seeking to understand women’s experiences in order to serve them better. This is research trying to understand women’s experiences in order to meet ‘national exclusive breastfeeding goals’.
So much for listening to women’s experiences rather than looking at the barriers to breastfeeding. Same old, same old here, I’m afraid: taking women’s stories and trying to use them to prop up breastfeeding advocacy, instead of believing women when they say that breastfeeding was not good for them. The authors frame infant feeding experiences as ‘complex’. How complex is ‘it hurt and I stopped breastfeeding’ or ‘it was inconvenient and I stopped breastfeeding’ or ‘I didn’t produce enough milk so I mix fed’? They don’t stop to consider that maybe breastfeeding advocacy has got it wrong and is failing to meet families’ needs.
It really is time to face reality. You cannot both serve the needs of families when it comes to feeding babies and seek to achieve ‘national exclusive breastfeeding goals’. It is time for families to stand up to breastfeeding advocacy and insist that healthcare providers serve us and not national breastfeeding goals. Our bodies, our babies, our families, our choice! It’s not complex at all!
This blog was adapted from a thread on Twitter.

